On the other hand, you can be sure that New York Presbyterian Queens (NYPQ) Hospital was even more grateful to get the talent and leadership skills of Casey, assistant professor in the School of Nursing since 2019 and owner of a diverse resume of education, experience and certification, most significantly as a Doctor of Nursing Practice (DNP) and Certified Registered Nurse Anesthetist (CRNA).
“I appreciate administrative leadership’s ability to be innovative and think outside the box during a crisis,” said Casey, who thanks Marieb College Dean and Professor Ann Cary, School of Nursing Director and Professor Anne Nolan and interim Provost James Llorens for making her mission of mercy possible.

With their blessing, Casey became another of the FGCU-affiliated or -trained healthcare professionals who have battled in the trenches of the pandemic, toiling inside COVID intensive-care units around the country — in her case, New York City. FGCU360 has asked these true soaring Eagles to share their personal experiences from the front lines of the health crisis.
Born in Celle, Germany, and, when not in Southwest Florida teaching students in the graduate-level Nurse Anesthesiology Program, residing in Clermont, Florida, Casey is married to sculptor Jim Casey. She also is on staff at TeamHealth Oak Hill Hospital in Spring Hill as a CRNA.
In the biography posted on her personal website, Casey describes her role as a university professor as the second phase of her nursing career — specifically, as an educator and nurse informaticist. Her first phase, concentrating on being an expert clinician in nurse anesthesia, began in 1993 as a registered nurse at Hughston Sports Medicine Hospital in Columbus, Georgia. It includes eight years as a Nurse Corps Officer in the U.S. Navy Reserve and working with Indian Health Services to serve Native American clients in rural areas, specifically the Sioux Nation in Rosebud, South Dakota.
Casey’s motivation? She credits her disabled brother and her mother for teaching her the values of persistence and leadership.
“I learned from my mother what a charismatic leader is,” Casey said. “Her leadership abilities enabled me to develop a strong sense of commitment, defend equal rights, embrace holistic values, and to strive to reach my fullest potential at all times. My professional goals echo these attributes.”
As for the second phase of her career — most prominently as a teacher at FGCU — Casey says she continues to use her “expertise and passion for nurse anesthesia and health information to engage students and promote better patient outcomes through the application of evidence-based care delivery.”
To be sure, Casey had to bring the knowledge she has gleaned and shared in both phases of her career to this latest challenge. Following are her reactions and reflections from that experience, which took place during most of the month of April as a Disaster Relief CRNA.
FGCU360: For you personally, what were the toughest things to deal with on the job?
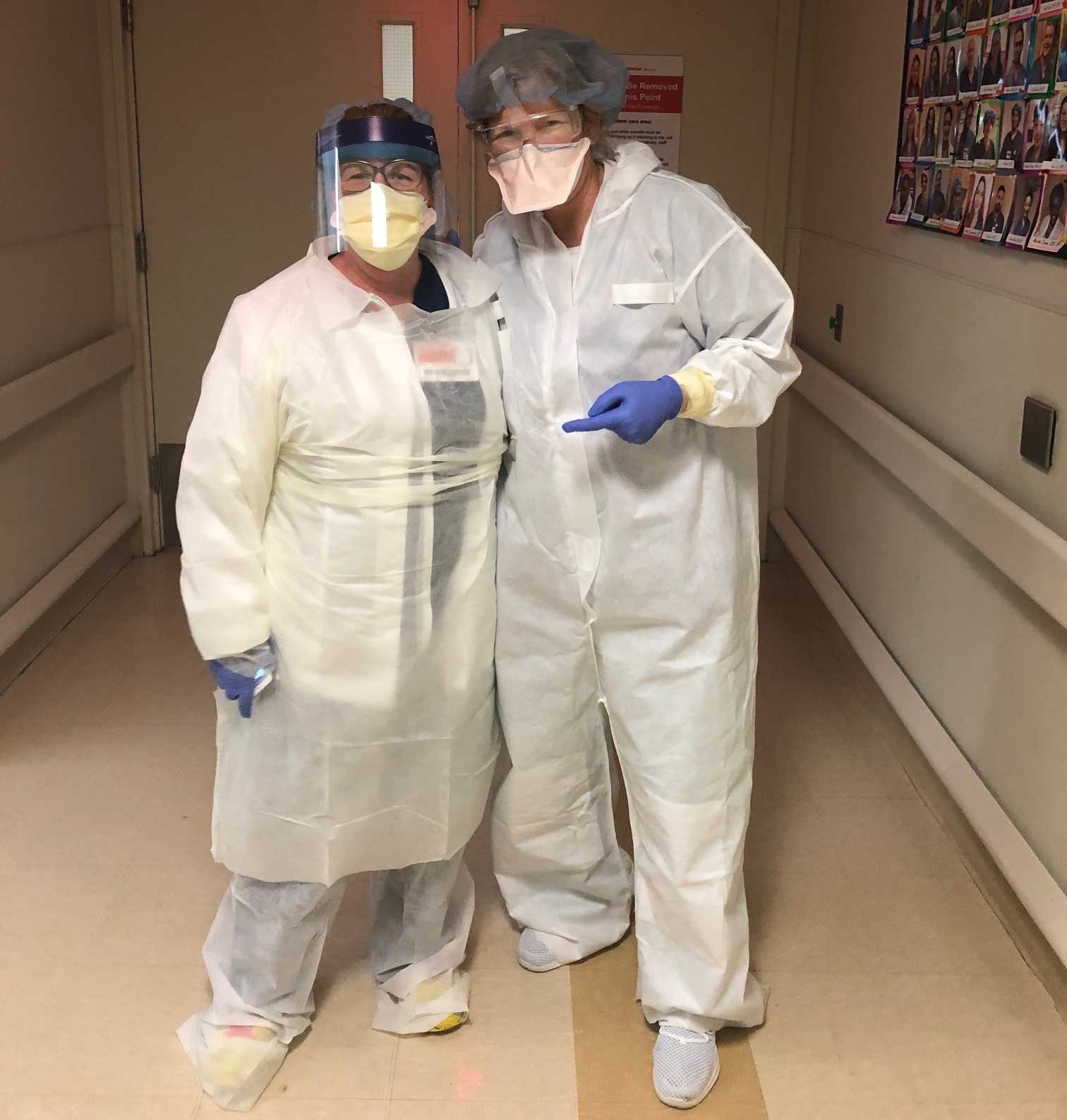
Imke Casey: Providing rapid response and emergency anesthesia services in a medical system that is overwhelmed with critically ill patients. An insufficient availability of personal protective equipment — N95 masks, disposable hooded overalls and face shields in particular — and being potentially exposed to the virus. Working with unsophisticated ventilators from the federal stockpile, specifically the LTV® 1200 versus in-house, contemporary ventilators such as the Servo-u mechanical ventilator.
On the human side, being at the brink of emotional and physical exhaustion after a 12-hour shift. Using Facetime and WhatsApp as the only means for families to express their encouragement and hope to their loved one. In many cases, families had to express their love and final goodbyes via these video-messaging platforms.
FGCU360: What positive developments did you see during the experience?
Imke Casey: It was amazing to see how healthcare workers from across the U.S., in all specialties, came together to fill the medical personnel shortage during the peak of the crisis at NYPQ. It necessitated the fastest interstate credentialing ever – New York Gov. Andrew Cuomo enacted Executive Order 202, with emergency credentialing procedures for healthcare staff. That means a process that usually takes four to six weeks is reduced to 24 hours. For example, I was asked to help on April 2, was credentialed, flew to New York on April 3, and was in the ICU at NYPQ providing critical-care services the next day.
I also met amazing colleagues from my home state of Florida there. And the NYPQ chief nursing officer deployed CRNAs and cross-trained ER and OR nurses to assist in critical-care settings.
FGCU360: In your opinion, what will be the action items that have to be addressed after this crisis has passed?
Imke Casey: There are many items that I feel need to be evaluated. First, can we expand the use of technology to engage family while providing palliative care or critical care? Should family be able to “see” their loved one while they are not are able to be physically present?
In terms of my profession (nurse anesthesia), I feel that we need to re-evaluate and potentially expand the scope of nurse anesthesia practice. While I have a strong background in emergency-, critical-care and rapid-response services (my prior Navy Reserve combat casualty-care training and solo anesthesia positions in rural America), the majority of CRNAs usually do not develop these skills, since the Council of Accreditation does not require nurse anesthesia students to rotate through the critical-care area or the emergency room.
I have been in contact with the CEO of the American Association of Nurse Anesthetists, Dr. Randall Moore, who also feels that this topic should be addressed by the AANA during a COVID-19 After Action Review. The goal would be to discuss the current nurse anesthesia scope of practice with educators and the Council of Accreditation related to needed emergency and critical-care services skills and training.

ABOUT THIS SERIES
FGCU360 contacted alums and faculty/staff members actively involved in the COVID-19 fight willing to share their personal story.
Previously:
- Sherri Parmar, nursing graduate working at Gulf Coast Medical Center in Fort Myers
- Kelly Goebel, assistant professor working at Naples Community Hospital
- Marylee Marre, nursing graduate working for the NYC Health + Hospitals system in New York City
- Shelby Miller, nursing graduate working at Tampa General Hospital
MESSAGES FROM MARIEB
“The economic and health impact our graduates have on not only our local communities but communities all over the United States is impressive. Marieb College and the School of Nursing is a major contributor to the health and welfare of our citizens. As we are now experiencing, health is tied directly to productivity in our economy and to social wellbeing. We are honored to produce nursing and health workforce graduates who are able to protect the health of the public.”
— Ann H. Cary, PhD, MPH, RN, FANP, FAAN
Dean and Professor, Marieb College of Health & Human Services
Chair, Board of Directors, American Association of Colleges of Nursing (2018-20)
Robert Wood Johnson Executive Nurse Fellow
“We are especially proud of our FGCU nursing alumni who are working on the frontlines of the COVID-19 response. We know they have outstanding skills and are emerging as leaders in nursing. We admire the resilience, initiative, dedication and fearlessness that set them apart in practice. On behalf of the FGCU School of Nursing faculty, staff and students, I would like to say thank you for your spirit and exceptional nursing care.”
— Anne Nolan, PhD, RN, FACN
Conner Professor in Nursing
Director, School of Nursing
Marieb College of Health & Human Services[/vc_column_text]